Table of Contents
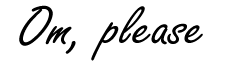
The human microbiome is a hidden and complex world of tens of thousands of microorganisms inhabiting our body. It’s no coincidence that it has recently become a focal point of scientific attention. This fantastic complex of bacteria, viruses, fungi, and other microbes living in the gastrointestinal tract, skin, and other tissues plays a crucial role in health.
With its numerous functions, the microbiome influences not only our physical state but also our mental status. Perhaps you are a professional in the field of medicine or psychology, or are you on the other side – suffering, looking for new ways to maintain your health?
This article will explore the relationship between the microbiome and autoimmune diseases, allergies, behavioral disorders, and even psychological traumas. We will combine scientific evidence and clinical experience with learning about the surprising ways the microbiome shapes and controls our health and well-being.
“You are what you eat.”
What is the human microbiome and why is it important for health?
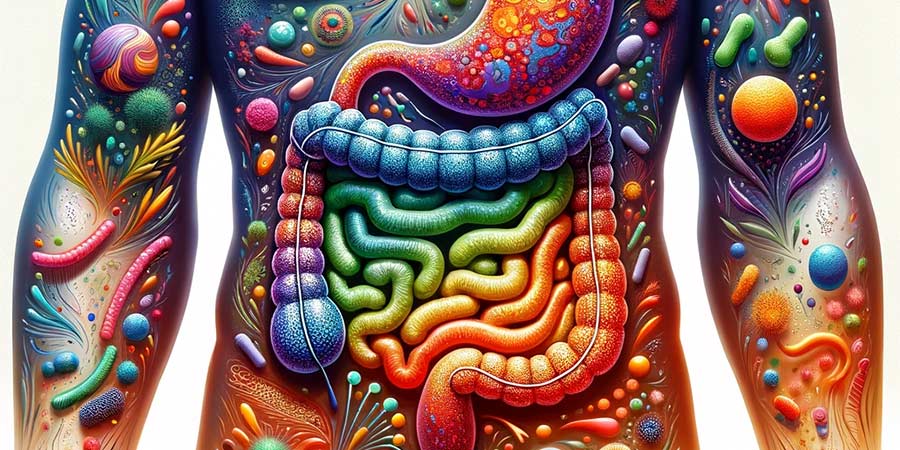
The microbiome is an incredibly diverse and rich world of microorganisms inhabiting our bodies. It involves billions of microorganisms, mainly bacteria, viruses, fungi, and parasites. This ecosystem is located in various body parts, with the predominant part concentrated in the gastrointestinal tract.
The microbes in this “micro-world” are represented in an extraordinary variety. It is believed that there are over 10,000 different species of bacteria in the human microbiome, divided into hundreds of billions of cells. Such a vast amount may sound scary, but if we look at our bodies under a microscope, they are teeming with life. Even on our eyelids and scalps, microorganisms live.
This extensive assortment is crucial because different types of bacteria perform diverse functions. The greater the diversity of bacteria in our ecosystem and the healthier the type, the better we feel.

These microorganisms help break down the foods we consume and produce vitamins and other essential nutrients. They regulate the immune system, protecting the body from infections and diseases. The microbiome also influences metabolism, helping to control body weight and energy balance.
Interestingly, the microbes are not in a constant composition – they renew and change constantly every 2 hours. The content of the microbiome depends on food, medication, emotional state, increased stress, and other external factors.
Many factors can disrupt the balance of the microbiome, such as poor diet, antibiotics, anxiety, and others. They can lead to various problems, including allergies, constipation, and even diseases like depression and diabetes. This dynamic shows we can influence our health through careful attention to the microbiome.
The Microbiome and Gluten Intolerance
In the past, allergies were usually associated with a weak immune system or heredity. However, recent scientific research reveals the connection between our microbiome and this severe health issue.
Based on new data, the question arises:
“How does the microbiome affect allergies, specifically, the most widely manifested allergies, such as gluten intolerance?”
The microbes in the gut actively participate in the breakdown of foods, including gluten, and can control our sensitivity to them. Consuming gluten can cause long-term changes in the microbiome, for instance, reducing the quantity of many important health-promoting bacteria.
Gluten Intolerance
80% of the immune system is influenced by the composition of gut bacteria and is associated with diffuse lymphoid intestinal tissue. If you suffer from gluten intolerance, the components into which gluten is broken down in the intestines signal the immune system through the lymphoid tissue, triggering an immune response through antibodies.
Some of the symptoms of pronounced sensitivity to gluten are upset stomach, bloated abdomen, and frequent visits to the toilet. With gluten intolerance, things become more serious. The antibodies that attack the broken-down gluten substances also attack the enzyme that breaks them down, called “tissue transglutaminase” (tTG).

Tissue Transglutaminase
The problem is that tissue transglutaminase is responsible for the microvilli’s health in the intestines’ walls. They are responsible for absorbing nutrients from food as they pass through the intestines, so if your tTG is attacked, they can’t function properly.
If this continues for a long time, the microvilli begin to break down. Consequently, nutrients cannot be properly absorbed. As a result, symptoms such as malnutrition, temporary constipation, diarrhea, and unexplained weight loss occur.
Prolonged consumption of gluten can cause permanent damage to the intestinal tissue and lead to a condition known as “leaky gut,” where the problem from the intestines spreads throughout the entire body.
Gluten can cause the intestinal cells to produce a protein called zonulin, which breaks down the bonds between the cells that make up the walls of the intestines. This means that everything that passes through the intestines – microbes, food particles, toxins, and the mentioned antibodies – can enter the bloodstream and spread throughout the body from there.
Once they reach other body parts, antibodies zealously attack everything around them. Hence, people with gluten intolerance develop health problems affecting organs seemingly unrelated to food, such as the thyroid gland, skin, and even the brain.
Gluten is one of the most prevalent allergens – an example of the microbiome’s connection to allergies and other diseases. Stress can also trigger a leaky gut, so the more informed you are, the easier you can chart a path to optimal health.
Leaky Gut
Leaky gut is a condition where intestinal tract walls become more permeable than average. What are the most common causes of the “leaky gut” condition?
Causes of Leaky Gut
- Poor diet and food choices. The intake of processed foods (ready meals, desserts, chips, snacks), high amounts of sugar, and foods containing colorings, enhancers, and preservatives can disrupt the integrity of the intestinal tract.
- Stress. Stress and anxiety can negatively affect the intestinal tract and contribute to intestinal permeability.
- Antibiotics. Antibiotics disrupt the gut ecosystem and increase the risk of a leaky gut. It’s not by chance that every doctor prescribes probiotics along with antibiotics.
- Unstable microbiome. An imbalance in the microbiome can increase intestinal permeability. A lack or insufficient intake of probiotics and prebiotics also increases the imbalance.
Symptoms of Leaky Gut
Symptoms of a leaky gut include digestive issues, constipation, fatigue, headache, brain fog, and even skin irritations (urticaria).
Treatment of Leaky Gut
- Healthy diet. It is necessary to avoid processed foods with preservatives and include foods rich in probiotics and prebiotics, which support the balance of the microbiome and reduce intestinal permeability.
- Stress management. Mindfulness and stress management techniques, such as yoga and meditation, can be beneficial for the overall recovery of the body, including gut health.
- Treating accompanying conditions. If leaky gut is associated with certain diseases, like Irritable Bowel Syndrome (IBS), their treatment can help, but it won’t be the sole sufficient solution without significant lifestyle changes.
Leaky gut is a complex problem; its treatment depends on the specific case and the factors causing it. Maintaining a healthy lifestyle and proper nutrition are the primary cure for this condition.
Undertaking intermittent fasting – abstaining from certain foods/ingredients or eating over a longer interval (e.g., “16-8” – 16 hours fasting + 8 hours eating interval), is an excellent strategy for restoring the microbiome’s and intestines’ health.
Fasting from gluten for a certain period – at least 1-3 months, while keeping a journal to observe how it affects the overall state – mindset, clarity of consciousness, allergy data after certain foods, monitoring gastrointestinal status, etc., is a good idea.
Microbiome and Autoimmune Diseases
The gastrointestinal tract’s microbiome actively regulates the immune system’s tolerance to its own cells and tissues. In a healthy organism, the immune system is tolerant of itself and does not react aggressively against them.
The microbiome maintains this balance by directing the immune system to recognize and respond effectively to foreign agents while not attacking its cells and tissues.
Suppose the microbiome is disrupted due to diet, antibiotics, stress, etc. In that case, there can be a disturbance in the immune system’s tolerance, and it may direct antibodies against its tissues, creating a predisposition for the development of autoimmune diseases.
Chronic inflammatory conditions are a common characteristic of many autoimmune diseases and increase the risk of their development. Disruption of the microbiome can interfere with regulating inflammatory responses in the body, leading the immune system towards chronic inflammatory processes.

Human Microbiome and Mental Health
The human microbiome is called “the second brain,” as it affects physical health and cognitive and emotional processes.
Microorganisms in the gastrointestinal tract produce neurotransmitters, such as serotonin and GABA, crucial to mood regulation and stress responses. These chemical signals are essential in controlling brain activity and emotional stability.
Chronic inflammation in the body often manifests as psychosomatic symptoms of depression and anxiety. Unique nerve connections between the gut and brain, called the “gut-brain axis,” provide a mechanism through which the microbiome communicates with the central nervous system. Irritable Bowel Syndrome (IBS), for example, is rooted in the psyche of the individual, not so much in the intestines.
Suppressed feelings, emotional traumas, and the inability of a person to find an outlet and solution to their problems, over time, lead to the development of various health issues in the body. As a rule, the individual’s most vulnerable system or organ is the first to suffer.
Regardless of whether a disease is caused by a psychological problem – an unresolved internal conflict, it should be treated not only by a psychologist but also by a medical specialist in the respective field. The psychological state is as important and real as its physical manifestation.
Caring for the microbiome is a means of maintaining optimal health. With its rich world of over 10,000 types of bacteria, it performs several vital functions, including maintaining the immune system, regulating inflammatory processes, and producing neurotransmitters affecting mood.
A holistic change in our lifestyle, thinking, and eating are excellent strategies for balancing and optimizing our health.
*This article is for informational purposes only. Before you begin a specific approach to nutrition and treatment of a condition, please always consult the respective health professional.